Connect With Us

Symptoms and Causes of Poor Foot Circulation

Poor circulation in the feet can lead to several uncomfortable symptoms that may interfere with daily life. Numbness and tingling are often the first signs, creating a pins and needles sensation that can spread across the feet or toes. Swelling may also occur as blood flow becomes sluggish, causing fluid to build up in the tissues. Feet may feel unusually cold, and skin color can appear pale or bluish. Common causes of poor circulation include diabetes, peripheral artery disease, smoking, and prolonged inactivity. Wearing tight shoes or sitting for long periods may also restrict blood flow. Identifying and addressing the underlying cause is important, as poor circulation can lead to serious complications. If you have any of the above symptoms, it is suggested that you consult a podiatrist who can offer you effective relief and management tips.
While poor circulation itself isn’t a condition; it is a symptom of another underlying health condition you may have. If you have any concerns with poor circulation in your feet contact Rahil Baxamusa, DPM of Illinois. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Peripheral artery disease (PAD) can potentially lead to poor circulation in the lower extremities. PAD is a condition that causes the blood vessels and arteries to narrow. In a linked condition called atherosclerosis, the arteries stiffen up due to a buildup of plaque in the arteries and blood vessels. These two conditions can cause a decrease in the amount of blood that flows to your extremities, therefore resulting in pain.
Symptoms
Some of the most common symptoms of poor circulation are:
- Numbness
- Tingling
- Throbbing or stinging pain in limbs
- Pain
- Muscle Cramps
Treatment for poor circulation often depends on the underlying condition that causes it. Methods for treatment may include insulin for diabetes, special exercise programs, surgery for varicose veins, or compression socks for swollen legs.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Causes Symptoms and Treatment for Poor Circulation in the Feet
The purpose of the body’s circulation system is to transport blood, oxygen, and nutrients throughout the body. A reduction of blood to a specific part of the body may cause one to experience symptoms of poor circulation. The most common causes of poor circulation in the feet are obesity, diabetes, and heart conditions such as peripheral artery disease (PAD). Common symptoms of poor circulation include tingling, numbness, throbbing, pain and muscle cramps.
Peripheral artery disease is a common cause of poor circulation in the legs. Symptoms of PAD are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. This pain tends to go away with rest and starts back up when you begin to walk. It is a condition that causes the blood vessels and arteries to become narrow. Although PAD is more common in adults over the age of 50, it may also occur in younger people. A similar condition called atherosclerosis causes arteries to stiffen up due to a buildup of plaque in the arteries and blood vessels.
Blood clots are also a common cause of poor circulation in the feet. Clots may obstruct blood vessels and if they occur in the legs, they may eventually lead to pain and discoloration. This occurrence is commonly known as deep vein thrombosis (DVT) and it may travel to the lungs. Varicose veins are another condition that may lead to poor circulation, and it is caused by incompetence of the valves in the veins. Women who are overweight are prone to developing this condition. Lastly, diabetes, which is correlated with poor blood sugar metabolism may lead to chronic poor circulation. Those with diabetes often suffer from cramping in the legs, calves, thighs and buttocks.
If you are looking for ways to avoid poor circulation there are some tips you can follow. One tip is to avoid sitting for too long. If you plan to sit down for a long period of time, you should try standing up occasionally, to improve your circulation. Another great way to avoid poor circulation is to exercise. Exercise is an excellent way to pump the heart and increase blood flow. Those who suffer from poor circulation should also avoid smoking, reduce their salt intake, and try to lose weight.
If you are experiencing symptoms from poor circulation in your feet, you should consult with your podiatrist to determine the best method for treatment for you. He or she may prescribe medication in addition to recommending specific lifestyle changes to improve your circulation.
Improving Balance Can Help Prevent Falls

As people age, changes in the feet, toes, and ankles can increase their risk of falling. Reduced joint flexibility, weaker muscles in the lower legs, and diminished sensation in the soles of the feet all contribute to poor balance. Common foot issues, such as bunions, hammertoes, or flat feet, may alter walking patterns and decrease stability. Limited ankle mobility also affects how the body responds to uneven surfaces or sudden shifts in direction. Even dry or thickened skin on the soles can affect grip and lead to slips. A podiatrist can evaluate these factors and provide care that supports balance. Options include suggesting supportive footwear, addressing biomechanical concerns, and prescribing custom orthotics to correct alignment. In some cases, foot or ankle surgery may be needed to correct structural problems that reduce stability. Strengthening the feet and ankles through guided exercises, along with proper foot care, can play an important role in fall prevention. If you are at risk for falling, it is suggested that you schedule an appointment with a podiatrist for an exam and suggestions for maintaining stability.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Rahil Baxamusa, DPM from Illinois. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.
The Three Grades of Ankle Sprains

An ankle sprain occurs when the ligaments that stabilize the ankle joint are stretched or torn, usually from rolling or twisting the foot. Ankle sprains are categorized into three grades, based on their severity. A Grade 1 sprain is mild and involves overstretched ligaments with minor swelling and tenderness. Most people can still walk, although with some discomfort. A Grade 2 sprain is considered moderate and includes only partial tearing of the ligament. This injury leads to more noticeable swelling, bruising, and joint instability. Walking may be painful, often causing a limp. A Grade 3 sprain is the most severe because it involves a complete ligament tear. This type of ankle sprain causes intense pain, pronounced swelling, and an inability to bear weight on the foot. A popping sound is sometimes heard at the time of injury. A podiatrist can assess your ankle injury, confirm the sprain grade, and provide the appropriate care. In severe cases, surgery may be necessary to restore stability. If you have sprained your ankle, it is suggested that you make an emergency appointment with a podiatrist for an exam and treatment.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact Rahil Baxamusa, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
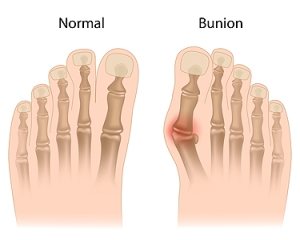
Managing Bunions
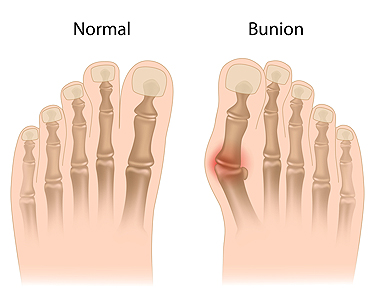
Bunions are bony bumps that form at the base of the big toe as the tip of the toe angles toward the second toe. Bunions are common among women, especially those who wear tight or high-heeled shoes, and older adults, whose joints may naturally weaken over time. Symptoms include pain, swelling, and redness surrounding the affected area, with the bunion becoming more noticeable as it grows. The condition can make walking uncomfortable and cause difficulty fitting into shoes. The primary cause of bunions is abnormal foot mechanics, often made worse by wearing ill-fitting shoes or having a family history of the condition. Arthritis or other joint conditions can also contribute to bunion development. A podiatrist can help by offering custom orthotics, padding, or shoe modifications to alleviate pain. In severe cases, surgery may be prescribed to correct the deformity. If you are have a painful bunion, it is suggested that you schedule an appointment with a podiatrist.
If you are suffering from bunion pain, contact Rahil Baxamusa, DPM of Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Symptoms and Treatment of High Arched Feet

High arches, or cavus foot, can cause significant pain due to the excessive pressure placed on the heel and the ball of the foot. People with high arches may experience pain when walking or standing, calluses from uneven weight distribution, curled toes, and ankle instability. Without proper support, high arches can contribute to an unsteady gait, increasing the risk of ankle sprains. A podiatrist may recommend custom orthotics to improve foot alignment and provide cushioning, foot pads to relieve pressure, or ankle braces to enhance stability. If non-surgical methods do not alleviate symptoms, surgery may be considered. For instance, a tendon transfer can help balance muscle function, while an osteotomy may be used to realign bones. In more severe cases, the plantar fascia can be partially cut to reduce arch tension and relieve pain caused by excessive tightness. Another option is fusing two or more bones in the foot to create a more stable structure. If you have high arches that cause discomfort, it is suggested that you schedule an appointment with a podiatrist for an exam, diagnosis, and treatment options, which may include surgery.
If you have any concerns about your feet, contact Rahil Baxamusa, DPM from Illinois. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Crystal Lake, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.